In the realm of chronic illnesses, Mast Cell Activation Syndrome (MCAS) is a complex disorder that is frequently the missing link in chronic mystery health issues. MCAS is gaining recognition in the medical community but still remains largely misunderstood by many. This article will delve into what MCAS is, its common causes, symptoms, diagnosis, and available treatment options.
What is Mast Cell Activation Syndrome?
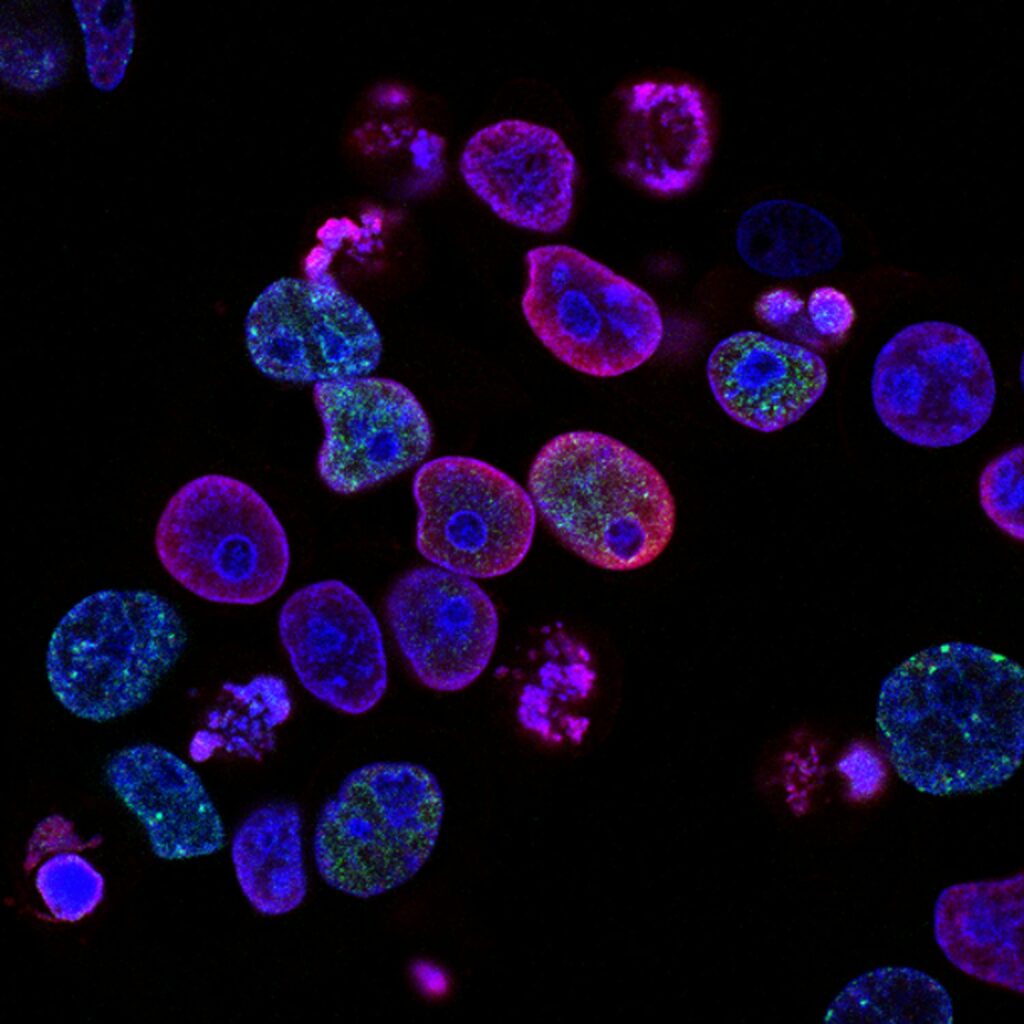
Mast cells, a crucial part of the immune system, are responsible for triggering allergic reactions by releasing various chemicals, including histamine, when the body detects a threat. In individuals with MCAS, these mast cells become hyper-reactive, and develop an abnormal response to triggers. This leads to excessive release of histamine and other inflammatory chemicals, contributing to a wide range of symptoms.
Common Causes of Mast Cell Activation Syndrome:
The exact cause of MCAS is unknown, and as with many chronic health syndromes, I suspect there are multiple contributing factors. However, several factors may contribute to its development, including:
- Genetics: Some research suggests a genetic predisposition to MCAS, indicating that certain individuals may inherit a propensity for abnormal mast cell function, and to develop histamine intolerance (difficulty breaking down excess histamine).
- Environmental Triggers: Exposure to environmental factors such as pollutants, toxins, infections, and certain medications can potentially exacerbate mast cell activation in susceptible individuals. There is also a theory that the body’s toxin threshold reaches a tipping point, and that mast cell disorders are related to environmental toxicity.
- Chronic Stress: Stress has been implicated in various immune-related disorders, and it’s thought to play a role in triggering or worsening MCAS symptoms. Certain hormones released in the presence of ongoing chronic stress can trigger mast cells.
- Viruses: Some individuals develop mast cell disorders after a viral trigger, such as influenza or Covid-19.
While these factors may contribute to the development of MCAS, it’s essential to recognize that the interplay between genetics, environment, and individual triggers can vary significantly from person to person.
Symptoms of MCAS:
The symptoms of MCAS are diverse and can mimic those of other conditions, making diagnosis challenging. Common symptoms include:
- Skin Reactions: Itching, hives (urticaria), flushing, and swelling (angioedema)
- Gastrointestinal Issues: Abdominal pain, diarrhea, nausea, vomiting, acid reflux, food sensitivities that seem to come-and-go, and more
- Neurological Symptoms: Headaches, migraines, brain fog, dizziness, vertigo, sensitivity to light, visual disturbances, and lightheadedness
- Psychiatric symptoms: Anxiety, panic attacks, depression, manic-like symptoms, obsessive compulsive symptoms, insomnia, and more
- Respiratory Symptoms: Wheezing, shortness of breath, nasal congestion, and throat swelling may occur. Anaphylaxis is also possible with MCAS.
- Cardiovascular Symptoms: Palpitations, low blood pressure (hypotension), tachycardia, and fainting spells (syncope)
- Constitutional symptoms: Fatigue, malaise, water retention, poor temperature control, chemical sensitivity, excess sweating
- Hormone Symptoms: Endometriosis, painful periods, feeling sick during ovulation, male and female infertility, interstitial cystitis
Diagnosis of MCAS:
Diagnosing MCAS can be challenging due to the nature of its symptoms and the lack of specific diagnostic tests. Many mast cell patients have a team of specialists and have been told there is no explanation for their symptoms. Healthcare providers typically rely on a combination of clinical history, physical examination, and laboratory tests to reach a diagnosis. Diagnosis includes:
- Symptom Assessment: A thorough evaluation of the patient’s medical history and symptomatology is essential in identifying patterns suggestive of MCAS. One key factor in diagnosis is that inflammatory symptoms present in two separate body systems in response to a trigger.
- Blood and Urine Tests: Measurement of serum tryptase levels, urinary histamine levels, and other mast cell mediators can provide valuable insights into mast cell activity. These tests need to be evaluated by a healthcare provider, as there is a high rate of false negatives depending on how the lab cared for the test samples.
- Antihistamine Response: Symptom improvement with treatment including antihistamines and mast cell stabilizers
While there is no definitive diagnostic test for MCAS, a comprehensive assessment by a knowledgeable healthcare provider is crucial in establishing an accurate diagnosis.
Mast Cell Activation Syndrome Triggers:
Unfortunately, just about anything can trigger mast cell degranulation when mast cells are overreactive.
Common triggers include:
- Mold/mycotoxins
- Stress (the client will often say, “I feel like I’m suddenly allergic to stress”)
- Hormone fluctuations
- Certain foods
- Temperature changes – excess heat and sometimes cold
- Exercise
- Heavy metals
- Acute and chronic illnesses
- Chemicals (fragrance, pesticides, food additives, etc)
- Surgery
- Lack of sleep
Treatment of MCAS:
The management of MCAS aims to alleviate symptoms, minimize triggers, and improve overall quality of life. Through the holistic lens, after MCAS is stable the aim is to reduce underlying factors that may be making the condition worse. Treatment strategies may include:
- Medications: Antihistamines, mast cell stabilizers, corticosteroids, and leukotriene inhibitors are commonly prescribed to control symptoms and prevent mast cell activation. In certain cases, immunotherapy or monoclonal antibody therapy is used.
- Trigger Avoidance: Identifying and avoiding triggers such as certain foods, medications, environmental allergens, and stressors can help reduce the frequency and severity of MCAS episodes.
- Dietary Supplements: Certain vitamins, minerals, and herbs can be helpful in correcting nutrient deficiencies, stabilizing mast cells, and reducing symptoms.
- Lifestyle Modifications: Stress management techniques, nervous system retraining, dietary modifications, and lifestyle adjustments may play a crucial role in managing MCAS symptoms and improving overall well-being.
Conclusion
Mast Cell Activation Syndrome is a complex and often perplexing disorder characterized by abnormal mast cell activation and the subsequent release of inflammatory mediators. Holistic and integrative medicine can offer many tools and solutions in managing this complex condition.